Introduction
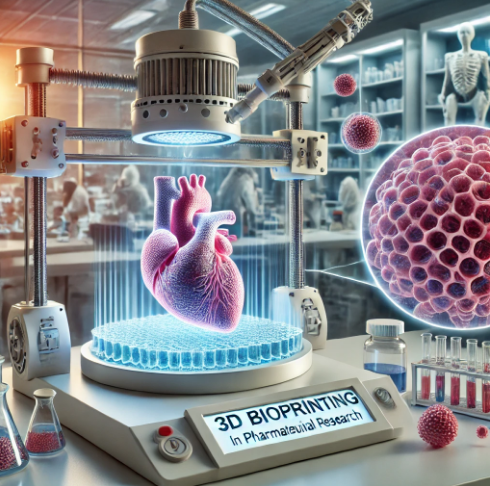
3D bioprinting, a branch of additive manufacturing, is rapidly transforming the field of pharmaceutical research and regenerative medicine. Unlike traditional 3D printing, which uses plastics and metals to create objects, 3D bioprinting uses bio-inks made from living cells to print tissues and organs layer by layer. This revolutionary technology has the potential to address a wide range of challenges in the pharmaceutical industry, from drug testing to personalized medicine, and may one day eliminate the need for organ donors.
In this article, we explore the mechanisms of 3D bioprinting, its applications in drug development and tissue engineering, the ethical challenges it poses, and its promising future in healthcare.
How 3D Bioprinting Works
At its core, 3D bioprinting mimics the body’s natural ability to build tissues. The process involves several key components:
- Bio-inks
Bio-inks are made from living cells and biocompatible materials such as hydrogels, which provide structural support and nutrients for cell growth. These bio-inks are carefully selected based on the type of tissue being printed. - Scaffolds
A scaffold acts as a framework that supports the cells as they grow and develop into functional tissue. The scaffold, made from biodegradable materials, provides mechanical strength to the bioprinted structure, allowing it to mimic the physical properties of native tissues. - Layer-by-Layer Printing
The bioprinter uses a computer-aided design (CAD) model to print the tissue one layer at a time. The bio-ink is deposited in precise locations, creating a 3D structure that mirrors the architecture of real tissues. The printed tissues are then incubated in controlled environments where they mature and become functional. - Bioprinters
There are different types of bioprinters, including inkjet, extrusion, and laser-assisted printers. Each type is suited to specific applications, such as printing soft tissues like skin or more complex structures like blood vessels.
Applications of 3D Bioprinting in Pharmaceuticals
The ability to create living tissues with 3D bioprinting has numerous applications in pharmaceutical research, particularly in drug development, personalized medicine, and regenerative therapies.
- Drug Testing and Development Traditional drug testing relies heavily on animal models and cell cultures, which often fail to accurately predict human responses. 3D bioprinting provides a solution by enabling the creation of human-like tissues and organ models for drug testing. For example:
- Organ-on-a-chip: Researchers can bioprint tiny, functional versions of human organs (such as liver or kidney tissue) to observe how a drug is metabolized or whether it causes toxicity.
- Precision drug testing: By using bioprinted tissues from specific patients, pharmaceutical companies can test how an individual’s unique genetic makeup might affect their response to a drug, leading to more effective and personalized treatments.
- Regenerative Medicine and Tissue Engineering 3D bioprinting is also a game changer for regenerative medicine. Scientists are already using it to create tissues that can replace damaged or diseased tissues in the body. Some promising examples include:
- Skin Grafts: 3D bioprinted skin tissues are being developed for burn victims, where personalized skin grafts can be produced to match a patient’s exact skin type.
- Heart Tissues: Researchers are working on creating patches of heart tissue that could be used to repair damage from heart attacks, reducing the risk of heart failure.
- Liver Constructs: 3D bioprinted liver constructs are already being used for testing the toxicity of drugs and, in the future, could potentially be used in transplantation.
- Personalized Drug Delivery Systems Another exciting application of 3D bioprinting is in creating customized drug delivery devices. These devices can be designed to match the patient’s anatomy or to deliver a drug in a controlled and sustained manner. This approach ensures that the patient receives the optimal dose of medication over time, improving treatment outcomes and reducing side effects.
Challenges and Ethical Considerations
While the potential of 3D bioprinting is vast, there are still several challenges and ethical issues to address before it can be widely used in clinical settings.
- Complexity of Functional Organs One of the biggest hurdles is the complexity of printing fully functional organs, like hearts or kidneys. While scientists have made significant progress in creating simple tissues such as skin, organs that require complex structures like blood vessels, nerves, and muscle tissue remain challenging. Research is ongoing, but fully bioprinted organs for transplantation may still be years away.
- Regulatory and Safety Concerns Regulatory bodies, such as the FDA, must develop guidelines to ensure the safety and efficacy of bioprinted tissues and organs. This includes standardizing the bioprinting process, ensuring the long-term stability of bioprinted tissues, and addressing potential risks like immune rejection.
- Ethical Issues The ability to bioprint human tissues raises ethical questions, particularly concerning the potential for organ bioprinting. Some fear that wealthy individuals could one day use this technology to “enhance” their bodies, leading to a form of biological inequality. There is also concern about the moral status of bioprinted tissues—particularly those that closely resemble human organs.
The Future of 3D Bioprinting in Pharmaceuticals
The future of 3D bioprinting in pharmaceutical research looks incredibly promising, with several exciting developments on the horizon.
- Organ Transplantation One of the most significant future applications of 3D bioprinting is in organ transplantation. Currently, there is a shortage of donor organs, and patients often wait years for transplants. In the future, 3D bioprinting could create organs on demand, eliminating the need for donors and reducing the risk of organ rejection.
- Combination with AI As 3D bioprinting continues to advance, combining it with artificial intelligence (AI) could lead to even more precise and efficient tissue creation. AI could help design better bioprinted structures and optimize the use of bio-inks, speeding up the process of tissue development.
- Bioprinting for Personalized Medicine Personalized medicine, where treatments are tailored to an individual’s genetic profile, could benefit greatly from 3D bioprinting. Scientists could bioprint tissues using a patient’s own cells, allowing for highly personalized drug testing, disease modeling, and even the creation of personalized organs or tissues for transplants.
Conclusion
3D bioprinting is revolutionizing the field of pharmaceutical research, offering new ways to test drugs, create personalized medicine, and even regenerate tissues. While there are still challenges to overcome, such as the complexity of creating fully functional organs, the potential of this technology is immense. As research progresses, 3D bioprinting could one day make it possible to bioprint organs on demand, radically changing the future of medicine.
References
- Murphy, S. V., & Atala, A. (2014). “3D bioprinting of tissues and organs.” Nature Biotechnology, 32(8), 773-785.
- Mandrycky, C., Wang, Z., Kim, K., & Kim, D. (2016). “3D bioprinting for engineering complex tissues.” Biotechnology Advances, 34(4), 422-434.
- Hospodiuk, M., Dey, M., Sosnoski, D., & Ozbolat, I. T. (2017). “The bioink: A comprehensive review on bioprintable materials.” Biotechnology Advances, 35(2), 217-239.