Introduction
Antibody-drug conjugates (ADCs) represent a promising new class of biopharmaceuticals that combine the specificity of monoclonal antibodies with the potent killing ability of cytotoxic drugs. Designed to deliver targeted cancer therapy, ADCs aim to improve the effectiveness of cancer treatments while minimizing damage to healthy cells. This article will explore how ADCs work, the advances in this field, current FDA-approved ADCs, challenges in development, and future directions for this technology.
Body
1. Mechanism of Action: How ADCs Work
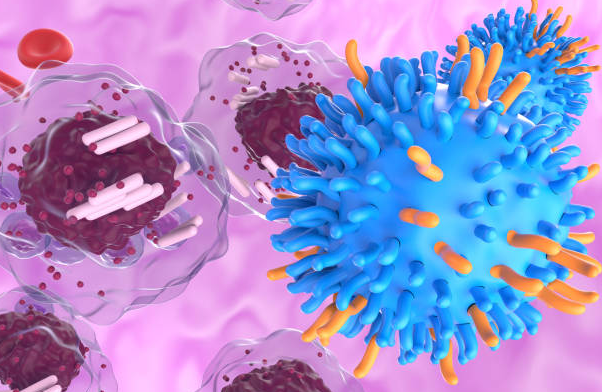
Antibody-drug conjugates are composed of three key components: a monoclonal antibody, a cytotoxic drug, and a linker that connects the two. The monoclonal antibody targets specific proteins expressed on the surface of cancer cells, ensuring the drug is delivered directly to the tumor. Once the ADC binds to the cancer cell, it is internalized, and the cytotoxic drug is released inside the cell, leading to cell death.
A. Monoclonal Antibodies as Targeting Agents
Monoclonal antibodies are engineered to recognize specific antigens or proteins found on the surface of cancer cells. This targeting capability ensures that the attached cytotoxic agent is delivered only to cells that express the antigen, reducing off-target effects and minimizing damage to healthy tissues.
B. Cytotoxic Drugs
The cytotoxic component of ADCs is often a potent chemotherapeutic agent that is too toxic to be delivered systemically. By linking it to the antibody, the cytotoxic drug is transported directly to the cancer cells, allowing for lower doses to be used while maintaining high efficacy.
C. The Linker
The linker in ADCs plays a crucial role in ensuring that the drug remains attached to the antibody until it reaches the tumor. Linker stability is critical to prevent the premature release of the cytotoxic drug, which could lead to unintended toxicity.
2. Current FDA-Approved Antibody-Drug Conjugates
The field of ADCs has grown significantly in recent years, with several FDA-approved therapies available for cancer treatment. Some of the most well-known ADCs include:
A. Trastuzumab Emtansine (Kadcyla)
Approved for the treatment of HER2-positive breast cancer, Kadcyla combines the monoclonal antibody trastuzumab with the cytotoxic drug DM1. This ADC targets the HER2 protein, which is overexpressed in certain types of breast cancer, allowing for targeted delivery of the chemotherapy agent.
B. Brentuximab Vedotin (Adcetris)
Used to treat Hodgkin lymphoma and systemic anaplastic large cell lymphoma, Adcetris targets CD30, a protein commonly found on the surface of these cancer cells. The drug consists of an anti-CD30 monoclonal antibody linked to monomethyl auristatin E (MMAE), a potent cytotoxic agent.
C. Enfortumab Vedotin (Padcev)
Padcev is used to treat advanced or metastatic urothelial cancer. This ADC targets Nectin-4, a protein commonly expressed in urothelial cancer cells. The cytotoxic payload is MMAE, which disrupts cell division and leads to cancer cell death.
3. Challenges in the Development of ADCs
While ADCs offer many advantages, their development presents significant challenges. These include ensuring the stability of the linker, avoiding off-target effects, and overcoming drug resistance in cancer cells.
A. Linker Stability
The stability of the linker between the antibody and the cytotoxic drug is crucial. If the linker is too stable, the drug may not be released at the tumor site, reducing efficacy. If the linker is too unstable, the drug may be released prematurely, causing toxicity to healthy cells.
B. Drug Resistance
Like other cancer therapies, ADCs are not immune to drug resistance. Cancer cells may develop mechanisms to evade ADCs, such as downregulating the expression of the target antigen or increasing drug efflux pumps that remove the cytotoxic agent from the cell.
C. Off-Target Effects
Although ADCs are designed to be highly specific, there is still the potential for off-target effects. The monoclonal antibody may bind to low levels of the target antigen present on healthy cells, leading to unintended toxicity.
4. Recent Advances in ADC Technology
Ongoing research in ADC technology is focused on improving the specificity, efficacy, and safety of these therapies. Some of the recent advances include:
A. New Linker Technologies
Researchers are developing more stable linkers that release the cytotoxic drug only in the tumor microenvironment, minimizing off-target effects. These new linkers are pH-sensitive, ensuring drug release only in the acidic environment of cancer cells.
B. Novel Cytotoxic Agents
The cytotoxic payloads used in ADCs are becoming increasingly diverse, with newer agents designed to overcome drug resistance mechanisms in cancer cells. These novel drugs are more potent and have unique mechanisms of action compared to traditional chemotherapies.
C. Bispecific Antibodies
Bispecific ADCs are being explored as a way to target multiple antigens simultaneously. By targeting two different proteins expressed on cancer cells, bispecific ADCs can increase specificity and reduce the likelihood of resistance.
5. Future Applications of ADCs in Cancer Therapy
The future of ADCs lies in expanding their use beyond traditional cancer therapies. Some potential future applications include:
A. Combination Therapies
ADCs are being studied in combination with other cancer therapies, such as immune checkpoint inhibitors and targeted therapies. These combinations may enhance the overall effectiveness of treatment and help overcome resistance mechanisms.
B. Personalized ADCs
As our understanding of cancer biology improves, it may become possible to develop personalized ADCs that are tailored to the unique characteristics of an individual’s tumor. This personalized approach could increase the specificity and efficacy of ADC treatment while reducing side effects.
C. Non-Cancer Applications
While ADCs are primarily used in cancer treatment, there is potential for their use in treating other diseases. Researchers are exploring the use of ADCs for autoimmune diseases, where targeted delivery of immunosuppressive agents could help reduce inflammation without compromising the entire immune system.
Conclusion
Antibody-drug conjugates represent a significant advancement in targeted cancer therapy, offering the potential to deliver highly potent cytotoxic drugs directly to cancer cells. With ongoing research and development, ADCs are becoming more effective and safer, expanding their potential applications in cancer and beyond. As new technologies emerge, ADCs will likely play an increasingly important role in the future of oncology treatment.
References:
- Chari, R. V. J., Miller, M. L., & Widdison, W. C. (2014). Antibody-drug conjugates: an emerging concept in cancer therapy. Nature Reviews Drug Discovery, 13(6), 447-464.
- Diamantis, N., & Banerji, U. (2016). Antibody-drug conjugates: an emerging class of cancer treatment. British Journal of Cancer, 114(4), 362-367.
- Thomas, A., Teicher, B. A., & Hassan, R. (2016). Antibody–drug conjugates for cancer therapy. The Lancet Oncology, 17(6), e254-e262.
- Lambert, J. M., & Berkenblit, A. (2018). Antibody–drug conjugates for cancer treatment. Annual Review of Medicine, 69, 191-207.